By Ladd McNamara, M.D.
 Everything on this website is for informational purposes only. This is not intended as medical advice. Consult your physician before using nutritional supplements. Please read full medical disclaimer via the link in the footer below.
Everything on this website is for informational purposes only. This is not intended as medical advice. Consult your physician before using nutritional supplements. Please read full medical disclaimer via the link in the footer below.
Many doctors tell patients to avoid vitamin and/or herbal supplements to avoid liver toxicity, particularly if one’s liver enzymes are elevated; but, is this the best advice? There are many vitamins, minerals, antioxidants, and herbal supplements that protect the liver from damage, and support normal liver function.
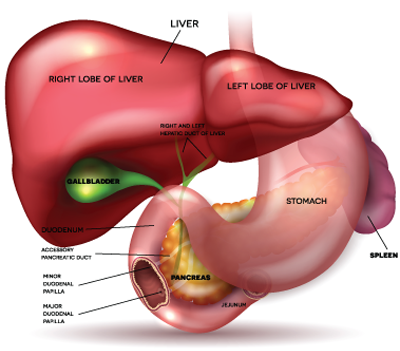
The liver is the workhorse of the digestive system. Everything you consume that is absorbed by the intestines, goes into the blood stream, and is filtered through the liver. The liver performs over 500 functions, which can be divided into three main categories– detoxification, synthesis, and storage. The liver can be negatively affected by drugs, alcohol, metals, environmental chemicals, viruses, and some herbs.
Main Liver Functions
- Detoxification of Toxic Metabolites from Blood
- Detoxification of Toxic Substances that are Consumed (alcohol, etc.)
- Synthesis of Cholesterol and Transport Proteins
- Synthesis of Triglycerides for Fuel
- Synthesis of Blood Proteins (albumin)
- Synthesis of Blood Clotting Proteins
- Synthesis of Angiotensinogen for Blood Pressure Control
- Synthesis and Metabolism of Hormones
- Synthesis of Proteins to Activate Immune System
- Synthesis of Enzymes
- Production of Bile for Emulsification of Fats
- Storage of Glucose as Glycogen
- Maintenance of Stable Blood Glucose Levels
- Storage of Fat Soluble Vitamins (A, D, E, K), and B12
- Recycling of Iron from Damaged Red Blood Cells
 The liver detoxifies toxins from food, drink, medications, drugs, and environmental chemicals, as well as toxins that accumulate in the blood as a result of metabolic processes. Ammonia is created from protein metabolism, and in elevated concentrations is quite toxic. The liver detoxifies ammonia, converting it into urea, and secreting it into the blood for excretion in the urine via the kidneys.
The liver detoxifies toxins from food, drink, medications, drugs, and environmental chemicals, as well as toxins that accumulate in the blood as a result of metabolic processes. Ammonia is created from protein metabolism, and in elevated concentrations is quite toxic. The liver detoxifies ammonia, converting it into urea, and secreting it into the blood for excretion in the urine via the kidneys.
The liver breaks down old and damaged red blood cells. Bilirubin is generated from the breakdown of hemoglobin, and the iron is stored in the liver for recycling. The liver produces bile which is stored in the gall bladder, until excreted into the duodenum for emulsification of dietary fats.
With liver damage, the detoxification process becomes inefficient or fails, liver enzymes then elevate, and ammonia and bilirubin build up in the blood. These toxic substances essentially poison the organs and cells of the body. Without liver recovery or a liver transplant, death is inevitable.
The liver synthesizes many different proteins, including albumin, the main protein in blood. Also, proteins are synthesized by the liver which are used as immune factors to reduce infections. In addition, the liver synthesizes proteins that are used as clotting factors to prevent hemorrhage.
The liver synthesizes fats, including triglycerides and cholesterol. The liver synthesizes high density and low density proteins for transporting the cholesterol through the blood. Cholesterol is needed for cell membranes, repair processes, and for the creation of hormones.
The liver stores fat-soluble vitamins, vitamins A, D, E, and K. Glucose is stored in the liver as glycogen, which is converted back into glucose when blood sugar drops. In this manner, the liver helps maintain normal blood glucose levels.
Liver Toxicity and Dysfunction
 With excess sugar intake and insulin resistance, fat accumulates in the liver, causing inflammation and toxicity. Liver enzymes elevate due to liver damage. This condition is known as nonalcoholic fatty liver disease, and it is the most common cause of liver dysfunction in the United States.
With excess sugar intake and insulin resistance, fat accumulates in the liver, causing inflammation and toxicity. Liver enzymes elevate due to liver damage. This condition is known as nonalcoholic fatty liver disease, and it is the most common cause of liver dysfunction in the United States.
Because the liver is taxed by toxic foods, drink, environmental toxins, and medications, let alone by high glycemic foods, insulin resistance, and stress hormones, it is important to protect the liver function with a high quality liver support supplement. Micronutrients are needed to optimize liver functions, and protect it from oxidative stress and inflammation.
Common Causes of Elevated Liver Enzymes (AST & ALT)
- Alcohol
- Acetaminophen (Tylenol)
- Medications (statin drugs, fluoxetine, aka, Prozac)
- Toxic hepatitis (from chemicals or drugs)
- Obesity
- Insulin resistance
- Hepatitis A, B, or C
- Heart failure
- Autoimmune hepatitis
- Celiac disease
- CMV or mononucleosis infections
- Hemochromatosis (iron overload)
- Wilson’s disease (copper metabolism disorder)
- Excessive Exercise on Day of Blood Work
Assessing Elevated Liver Enzymes
 Doctors treating patients with elevated liver enzymes will often wrongly accuse a quality liver support supplement of exacerbating liver toxicity. The usual recommendation is to stop all vitamins, minerals, and antioxidants. Unfortunately, the very micronutrients that can help protect the liver are withdrawn. A quality liver support supplement will benefit a damaged liver by protecting it from further oxidative stress, inflammation, and toxicity.
Doctors treating patients with elevated liver enzymes will often wrongly accuse a quality liver support supplement of exacerbating liver toxicity. The usual recommendation is to stop all vitamins, minerals, and antioxidants. Unfortunately, the very micronutrients that can help protect the liver are withdrawn. A quality liver support supplement will benefit a damaged liver by protecting it from further oxidative stress, inflammation, and toxicity.
Although some herbal supplements may need to be stopped in the presence of elevated liver enzymes, several micronutrient and herbal supplements are actually the best thing that can be taken. Those include co-enzyme Q10, alpha lipoic acid, grape seed extract, milk thistle extract, and many others.
If a person starts a quality nutritional supplement program, and is later found to have elevated liver enzymes, it must not be assumed that toxicity is due to the supplements. It is most likely due to some other cause, which needs to be explored.
The two most commonly elevated liver enzymes of concern are aspartate aminotransferase (AST) and alanine aminotransferase (ALT). The laboratory range for normal AST is between 10 to 30 units per liter and ALT between 7 to 56 units per liter. Mild elevations are generally considered to be 2 – 3 times higher than the upper normal range.
About 1% to 9% of asymptomatic patients have elevated enzyme levels when routinely screened with standard liver function panels. With mildly elevated liver enzyme tests, which is less than 4 times the upper limit of normal, often nothing but making minor lifestyle changes and following the enzyme levels need to be done.
 For example, if one’s AST is 90 U/L, simple inquiry regarding use of herbal supplements, recent alcohol ingestion, the use of medications such as Tylenol, statin drugs, or street drugs, excessive sugar intake, or significant exercise within a day prior to the blood draw can reveal possible causes. There are many other causes of elevated liver enzymes, so if none of the above are implicated, it still does not make sense to recommend stopping quality nutritional supplements, including a liver support supplement.
For example, if one’s AST is 90 U/L, simple inquiry regarding use of herbal supplements, recent alcohol ingestion, the use of medications such as Tylenol, statin drugs, or street drugs, excessive sugar intake, or significant exercise within a day prior to the blood draw can reveal possible causes. There are many other causes of elevated liver enzymes, so if none of the above are implicated, it still does not make sense to recommend stopping quality nutritional supplements, including a liver support supplement.
Lab work can be repeated in 8 weeks, and the patient can be encouraged to follow a low-glycemic diet, avoid alcohol (or minimize it, and not drink it within 48 hours of the next blood draw), and not take Tylenol within 48 hours of the next blood draw. If the liver enzymes remain elevated, then further evaluation should be done. The most common liver disorder is nonalcoholic fatty liver disease, often due to insulin resistance and/or obesity, which is one of the many factors that should be considered when liver enzymes are elevated.
Quality vitamins, minerals, and a high-quality liver support supplement do not cause elevation of liver enzymes, particularly at the suggested doses found on the bottle; and therefore, they can be continued in the presence of elevated liver enzymes. In fact, with a high quality liver support supplement, there is no liver toxicity even at ten times the daily dose suggested on the bottle.
A Quality Liver Support Supplement
A high quality liver support supplement will provide multiple micronutrients which are both safe and effective. The micronutrients will support the numerous liver functions, such as detoxification of toxic metabolites (particularly phase 2 liver detoxification, which is the elimination of the most toxic metabolites produced by phase 1 detoxification). Liver support will be reflected in normalization (or improvement) of liver enzymes.
 Nonalcoholic fatty liver disease (NAFLD), also known as hepatic steatosis, which leads to the accumulation of fat within the liver. NAFLD is mostly associated with obesity, high-glycemic diets, and insulin resistance. It can occur without obesity. NAFLD involves liver inflammation, dysfunction, and elevated liver enzymes, and in the worst case scenario, it can result in death.
Nonalcoholic fatty liver disease (NAFLD), also known as hepatic steatosis, which leads to the accumulation of fat within the liver. NAFLD is mostly associated with obesity, high-glycemic diets, and insulin resistance. It can occur without obesity. NAFLD involves liver inflammation, dysfunction, and elevated liver enzymes, and in the worst case scenario, it can result in death.
Daily use of a liver support supplement with multiple antioxidants will help reduce inflammation within the liver. The micronutrients will protect the liver from oxidative stress, which is increased in those with liver dysfunction, such as cirrhosis, hepatitis, and alcoholic and nonalcoholic fatty liver disease. The micronutrients will also benefit every other tissue and cell of the body, as the antioxidants in the liver support supplement are hardly restricted to entering the liver.
Micronutrients included in a quality liver support supplement—
- Milk Thistle Extract (silymarin)
- N-Acetyl-L-Cysteine (NAC)
- Alpha Lipoic Acid (ACA)
- Broccoli Extract
- Green Tea Extract (EGCG)
- Olive Extract
- Turmeric Extract (curcumin)
Below is a cursory overview of the benefits and safety of the micronutrients provided in a quality liver support supplement. The benefits of the antioxidants and cited references are not meant to be comprehensive in this article.
N-Acetyl-L-Cysteine (NAC)

N-Acetyl-L-Cysteine (NAC) is given intravenously to patients who present to emergency room with a Tylenol overdose. NAC counteracts the toxic effect of acetaminophen, as well as other drugs and environmental toxins. NAC directly provides antioxidant protection. It also is converted in the body to glutathione, one of the most powerful antioxidants known. Increasing glutathione within the liver is very effective in providing protection from oxidative stress and inflammation. NAC also protects the kidneys, brain, lungs, intestines, prostate, breasts, and every other tissue and cell in the body.
NAC regulates the important brain neurotransmitter, glutamate. Glutamate is involved in a broad range of learning, behavior, and memory functions. In Alzheimer’s disease and Parkinson’s disease patients, supplementation with generous doses of NAC improves both dopamine function and disease symptoms. (1, 2)
N-Acetyl-L-Cysteine also supports the immune system, possibly reducing the risk of cancer. Studies have shown the ability of NAC to induce apoptosis, or cancer cell death. (3, 4) It also blocks cancer cell duplication and proliferation.
NAC does not elevate liver enzymes; quite the opposite. It protects the liver, and together with the other micronutrients, will bring about the normalization of liver enzymes as liver dysfunction improves.
Alpha Lipoic Acid
Alpha lipoic acid is well known for its therapeutic role in the treatment of insulin resistance and diabetic polyneuropathy. It is used to treat alcohol-induced liver and nerve damage, mushroom poisoning, metal toxicity, carbon tetrachloride poisoning, and insulin resistance.
Alpha lipoic acid helps reduce cardiovascular disease, by protecting arterial endothelial cells, as well as by lowering blood pressure in those with hypertension. (5, 6) ALA reduces the risk for cardiovascular disease among diabetics. (7)
In a study among pregnant women with gestational diabetes, 100 mg/day of alpha lipoic acid was shown to reduce glucose levels and improve liver function, as shown by improved liver enzymes. (8) Animal studies have shown that alpha lipoic acid prevents fatty liver disease. (9)
Due to ALA’s effectiveness in reducing insulin resistance, and protection of fatty liver disease, it is an important micronutrient as part of a liver support supplement.
Curcumin (Turmeric Extract)

The benefits of curcumin seem unlimited, as an increasing number of studies are published revealing its benefits in the prevention and possible treatment of cancer, as wells as liver disease, heart disease, diabetes, neurological diseases, and pulmonary diseases. (10)
The number of studies showing the health benefits of curcumin is so voluminous that it is unreasonable for me to reference them all. A simple pubmed search of curcumin will quickly remove any doubt even from the most skeptical physician.
Curcumin enhances phase 2 detoxification, and in animal studies, has been shown to attenuate hepatic pathological damage, and decrease serum ALT and AST levels. (11) In a short-term randomized controlled study of curcumin administered to patients with nonalcoholic fatty liver disease, 1000 mg/day of curcumin was found to be safe and well tolerated. Curcumin was shown to improve liver fat percentage in fatty liver disease, and reduce liver enzyme levels. (12)
Broccoli Extract
Broccoli extract (containing at least sulforaphane and glucoraphanin), is a powerful antioxidant, that appears to reduce the risk of several types of cancers, as well as inhibit ulcer-causing Helicobacter pylori bacteria, and lower LDL cholesterol. It also protects against liver damage and dysfunction.
Studies have shown benefits of glucoraphanin from broccoli extract for reducing obesity-induced inflammation and insulin resistance. Broccoli extract also helps reduce fatty liver disease. (13) Broccoli extract also helps improve glucose control in type 2 diabetics. (14)
Broccoli extract protects against liver damage, and helps improve liver function, as seen with improved liver enzyme levels. (15)
Olive Extract
 Olive extract (containing polyphenolic antioxidants, such as oleuropein, oleanolic acid, and maslinic acid), has been shown to provide numerous health benefits, including reducing the risk of cardiovascular disease, cancers, neurological diseases, liver disease, and skin disorders. The micronutrients found in olive extract improve arterial elasticity, and reduce triglyceride levels and oxidized LDL cholesterol. (16) Olive extract reduces the neurological changes seen within neurons that are associated with Parkinson’s disease. (17)
Olive extract (containing polyphenolic antioxidants, such as oleuropein, oleanolic acid, and maslinic acid), has been shown to provide numerous health benefits, including reducing the risk of cardiovascular disease, cancers, neurological diseases, liver disease, and skin disorders. The micronutrients found in olive extract improve arterial elasticity, and reduce triglyceride levels and oxidized LDL cholesterol. (16) Olive extract reduces the neurological changes seen within neurons that are associated with Parkinson’s disease. (17)
Olive extract is beneficial for protecting against cancers. It has been shown to inhibit cancer cell proliferation, and induce apoptosis in colon cancer cells. (18, 19) In the animal model, olive extract has been shown to inhibit the development of liver cancer. (20)
Olive extract helps protect the liver, and improve liver enzyme levels. In animal studies with known hepato-toxic medications or chemicals (fluoxetine, doxorubicin, carbon tetrachloride), olive extracts were shown to protect against liver damage, and normalize liver enzyme levels. (21 – 23) Olive extract has been shown to specifically help prevent and improve fatty liver disease. (24, 25)
Milk Thistle Extract
Many doctors might see the herb milk thistle extract (silymarin) on the ingredient list of a high quality liver support supplement, and have a negative knee-jerk reaction. However, milk thistle extract supports liver function and protects against liver damage. (26)

Many doctors treating a patient with elevated liver enzymes, might evaluate a liver support supplement, and upon seeing the herb, milk thistle extract (silymarin) on the ingredient list, have a negative knee-jerk reaction, and recommend discontinuance of the supplement. Unfortunately, this is counter to the scientific research, which shows that milk thistle extract supports liver function, protects against liver damage, and improves liver enzyme levels. (26)
Milk thistle extract (containing silymarin and silibinin) is an antioxidant that improves liver function, including supporting detoxification functions. In a meta-analysis of studies involving over 10,000 patients with liver disease, administration of milk thistle extract (silymarin) was shown to reduce serum levels of the liver enzymes alanine aminotransferase (ALT), aspartate aminotransferase (AST) and gamma glutamyl transpeptidase (γGT), albeit, minimally. (27) Despite the minimal decrease in enzymes, milk thistle extract was shown not to cause an elevation of liver enzymes, and therefore, a milk thistle extract supplement would not need to be stopped in the presence of liver disease.
The bio-availability of commercially available milk thistle extract varies considerably. The potency and purity varies as well. These factors greatly affect the effectiveness of milk thistle extract in protecting and supporting the liver. These are a few possible reasons for discrepancies in the various studies. This is why I only advise the use of a high-quality liver support supplement.
Milk thistle extract, and the other micronutrients mentioned in this article, are all beneficial to use in the presence of various liver disorders, particularly fatty liver disease, other chronic liver diseases, liver cirrhosis, and hepatocellular carcinoma. All antioxidants protect against oxidative stress and inflammation, and work everywhere in the body. Through modulation of the inflammatory cascade and supporting the immune system, liver damage is minimized from all types of liver disorders– alcoholic or nonalcoholic liver disease, infectious hepatitis, toxic substances, etc.
In regard to alcohol, silymarin is able to increase liver cellular vitality and reduce both lipid peroxidation and cellular necrosis. (28) Importantly, a silymarin/silybin-containing supplement is able to reduce non-alcoholic fatty liver disease. (29)
Green Tea Extract
Doctors are being encouraged to inquire about the use of green tea extract supplements when they find elevated liver enzymes on a patient’s lab report. Unfortunately, other than hearing that supplements containing green tea extract are “toxic” to the liver, most doctors are unaware of the protective benefits of green tea extract to the liver, let alone the numerous other benefits provided by this remarkable micronutrient.

Indeed, there are reports of elevated liver enzymes among people using high-dose green tea extract supplements for weight loss. Green tea extract raises metabolism and reduces appetite. For this reason, some people eager to lose weight quickly, tend to over-do it with such weight-loss supplements. Despite this concern, to date, it appears that only 7 people have experienced any significant liver toxicity. And, it is unclear whether green tea extract alone, or in conjunction with other factors, caused liver damage.
We don’t know if the seven people who had liver toxicity were also taking certain medications or drinking alcohol, which are known to elevate liver enzymes. Could the combination of liver-toxic substances and high-dose green tea extract be the problem? Either way, if we go ahead and assume the 7 cases were solely due to high-dose (> 1000 mg/day) of green tea extract, the high-quality liver support supplement that I recommend, provides only a dose of 45 mg/day. I do suggest taking up to 180 – 200 mg of green tea extract, which is well below the dose that physician researchers suggest to avoid.
Studies actually show that green tea extract (EGCG) may help prevent and reverse nonalcoholic fatty liver disease. In one study, patients with nonalcoholic fatty liver disease were given 500 mg/day of concentrated green tea powder extracts. At the end of 90 days, the patients were found to have improved liver function tests. (30) In another study among patients with nonalcoholic fatty liver disease, 500 mg/day of green tea extract was shown to significantly improve metabolic, chemical, inflammatory, and radiological parameters. (31)
Multiple studies show that green tea extract is both safe and effective. The studies show that even doses of green tea extract up to 700 mg per day does not cause an elevation of liver enzymes. (32, 33) Even more so, the European Food Safety Authority (EFSA) concluded that “there was no indication of liver injury for doses below 800 mg/day from green tea supplements.”
Clearly, the liver benefits of green tea extract outweigh any theoretical risks, as long as the daily dose remains below 800 mg/day. Therefore, a high-quality liver support supplement that provides only 45 mg in a daily dose, along with the other micronutrients mentioned in this article, would have only benefits on the liver; even if taken at ten-times the dose.
A list of green tea extract’s proven benefits–
 • Liver support (help with detoxification process, and reduction of fatty liver disease)
• Liver support (help with detoxification process, and reduction of fatty liver disease)
• Reduction of blood pressure
• Heart support (reduction of cardiovascular disease and blood pressure)
• Neuroprotection (e.g., Alzheimer’s disease, Parkinson’s disease, Multiple Sclerosis)
• Eye support (particularly glaucoma)
• Bone support
• Fat metabolism
• Immune support (protection against cancers, including liver cancer)
• Chemo-prevention against many cancers, including cancer of the liver
• Anti-HPV (reduction of cervical dysplasia and cervical cancer)
Conclusion
Although a high-quality liver support supplement is marketed for the liver, the various micronutrients benefit the body far beyond protecting and supporting the liver. The collective benefits of the micronutrients are so significant, that everyone, not just those with liver disease, should highly consider taking the high-quality liver support supplement daily. Those with any type of liver disease should consider taking the high-quality liver support supplement at double or triple the daily dose.
If you have fatty liver disease, insulin resistance, diabetes (type 1 or type 2), high cholesterol, high triglycerides, hepatitis, exposure to toxic substances (including alcohol), gall bladder disorders, liver cancer, any cancer, high blood pressure, cardiovascular disease, obesity, Alzheimer’s disease, Parkinson’s disease, or are taking a statin drug, using Tylenol, or are concerned about any of these issues, then definitely consider taking this important high-quality liver support supplement daily, at two -to-three times the suggested dose …for life. (Discuss with your doctor first.)
If you have any interest in my nutritional supplement protocols for elevated liver enzymes, nonalcoholic fatty liver disease, hepatitis, cirrhosis, diabetes, insulin resistance, or any other health condition, please consider becoming a member of my Dr. Ladd VIP Program.
Everything on this website is for informational purposes only. It is not intended as medical advice. Consult your physician before using nutritional supplements. Please read full medical disclaimer via the link in the footer below.
References
- Mokhtari V, et al. A Review on Various Uses of N-Acetyl Cysteine. Cell J. 2017 Apr-Jun;19(1):11-17.
- Tardiolo G, et al. Overview on the Effects of N-Acetylcysteine in Neurodegenerative Diseases. 2018 Dec 13;23(12).
- Guan D, et al. N-acetyl cysteine and penicillamine induce apoptosis via the ER stress response-signaling pathway. Mol Carcinog. 2010 Jan;49(1):68-74.
- Li J, et al. N-acetyl cysteine inhibits human signet ring cell gastric cancer cell line (SJ-89) cell growth by inducing apoptosis and DNA synthesis arrest. Eur J Gastroenterol Hepatol. 2007 Sep;19(9):769-74.
- Tromba L, et al. Effect of Alpha-Lipoic Acid Supplementation on Endothelial Function and Cardiovascular Risk Factors in Overweight/Obese Youths: A Double-Blind, Placebo-Controlled Randomized Trial. Nutrients. 2019 Feb 12;11(2).
- Boccardi V, et al. Elevated blood pressure reduction after α-lipoic acid supplementation: a meta-analysis of randomized controlled trials. J Hum Hypertens. 2019 Feb 11.
- Dworacka M, et al. New arguments for beneficial effects of alpha-lipoic acid on the cardiovascular system in the course of type 2 diabetes. Eur J Pharm Sci. 2018 May 30;117:41-47.
- Aslfalah H, et al. Reduction in maternal serum values of glucose and gamma-glutamyltransferase after supplementation with alpha-lipoic acid in women with gestational diabetes mellitus. J Obstet Gynaecol Res. 2019 Feb;45(2):313-317.
- Sena CM, et al. Lipoic Acid Prevents High-Fat Diet-Induced Hepatic Steatosis in Goto Kakizaki Rats by Reducing Oxidative Stress Through Nrf2 Activation. Int J Mol Sci. 2018 Sep 11;19(9).
- Xu XY, et al. Bioactivity, Health Benefits, and Related Molecular Mechanisms of Curcumin: Current Progress, Challenges, and Perspectives. Nutrients. 2018 Oct 19;10(10).
- Xie YL, et al. Curcumin attenuates lipopolysaccharide/d-galactosamine-induced acute liver injury by activating Nrf2 nuclear translocation and inhibiting NF-kB activation. Biomed Pharmacother. 2017 Jul;91:70-77.
- Panahi Y, et al. Efficacy and Safety of Phytosomal Curcumin in Non-Alcoholic Fatty Liver Disease: A Randomized Controlled Trial. Drug Res (Stuttg). 2017 Apr;67(4):244-251.
- Xu L, et al. Glucoraphanin: a broccoli sprout extract that ameliorates obesity-induced inflammation and insulin resistance. Adipocyte. 2018;7(3):218-225.
- Axelsson AS, et al. Sulforaphane reduces hepatic glucose production and improves glucose control in patients with type 2 diabetes. Sci Transl Med. 2017 Jun 14;9(394).
- Kikuchi M, et al. Sulforaphane-rich broccoli sprout extract improves hepatic abnormalities in male subjects. World J Gastroenterol. 2015 Nov 21;21(43):12457-67.
- Pais P, et al. Impact of a Proprietary Standardized Olive Fruit Extract (SOFE) on Cardio-Ankle Vascular Index, Visual Analog Scale and C-Reactive Protein Assessments in Subjects with Arterial Stiffness Risk. Drugs R D. 2016 Dec;16(4):355-368.
- Mohammad-Beigi H, et al. Oleuropein derivatives from olive fruit extracts reduce α-synuclein fibrillation and oligomer toxicity. J Biol Chem. 2019 Jan 17.
- Juan ME, et al. Olive fruit extracts inhibit proliferation and induce apoptosis in HT-29 human colon cancer cells. J Nutr. 2006 Oct;136(10):2553-7.
- Juan ME, et al. Antiproliferative and apoptosis-inducing effects of maslinic and oleanolic acids, two pentacyclic triterpenes from olives, on HT-29 colon cancer cells. Br J Nutr. 2008 Jul;100(1):36-43.
- Amereh Z, et al. Cancer chemoprevention by oleaster (Elaeagnus angustifoli L.) fruit extract in a model of hepatocellular carcinoma induced by diethylnitrosamine in rats. EXCLI J. 2017 Jul 18;16:1046-1056.
- Elgebaly HA, et al. Olive oil and leaf extract prevent fluoxetine-induced hepatotoxicity by attenuating oxidative stress, inflammation and apoptosis. Biomed Pharmacother. 2018 Feb;98:446-453.
- Kumral A, et al. Effect of olive leaf extract treatment on doxorubicin-induced cardiac, hepatic and renal toxicity in rats. Pathophysiology. 2015 Jun;22(2):117-23.
- Eidi A, et al. Hepatoprotective effects of Portulaca oleracea extract against CCl4-induced damage in rats. Pharm Biol. 2015 Jul;53(7):1042-51.
- Vergani L, et al. Polyphenolic extract attenuates fatty acid-induced steatosis and oxidative stress in hepatic and endothelial cells. Eur J Nutr. 2018 Aug;57(5):1793-1805.
- Omagari K, et al. Olive leaf extract prevents spontaneous occurrence of non-alcoholic steatohepatitis in SHR/NDmcr-cp rats. Pathology. 2010 Jan;42(1):66-72.
- Shaker E, et al. Silymarin, the antioxidant component and Silybum marianum extracts prevent liver damage. Food Chem Toxicol. 2010 Mar;48(3):803-6.
- de Avelar CR, et al. Effect of silymarin on biochemical indicators in patients with liver disease: Systematic review with meta-analysis. World J Gastroenterol. 2017 Jul 21;23(27):5004-5017.
- Federico A, et al. Silymarin/Silybin and Chronic Liver Disease: A Marriage of Many Years. Molecules. 2017 Jan 24;22(2).
- Pais P, D’Amato M. In vivo efficacy study of milk thistle extract (ETHIS-094™) in STAM™ model of nonalcoholic steatohepatitis. Drugs R D. 2014 Dec;14(4):291-9.
- Pezeshki A, et al. The Effect of Green Tea Extract Supplementation on Liver Enzymes in Patients with Nonalcoholic Fatty Liver Disease. Int J Prev Med. 2016 Feb 1;7:28.
- Hussain M, et al. Therapeutic benefits of green tea extract on various parameters in non-alcoholic fatty liver disease patients. Pak J Med Sci. 2017 Jul-Aug;33(4):931-936.
- Hu J, et al. The safety of green tea and green tea extract consumption in adults – Results of a systematic review. Regul Toxicol Pharmacol. 2018 Jun;95:412-433.
- Dekant W, et al. Safety assessment of green tea based beverages and dried green tea extracts as nutritional supplements. Toxicol Lett. 2017 Aug 5;277:104-108.
Everything on this website is for informational purposes only. It is not intended as medical advice. Consult your physician before using nutritional supplements. Please read full medical disclaimer via the link in the footer below.