by Ladd McNamara, M.D.
 Most doctors are hyper-focused on lowering LDL cholesterol levels, usually with the use of statin drugs. HDL cholesterol is called the “good cholesterol,” and LDL cholesterol is dubbed, “the bad cholesterol.” However, there is nothing inherently bad about LDL cholesterol.
Most doctors are hyper-focused on lowering LDL cholesterol levels, usually with the use of statin drugs. HDL cholesterol is called the “good cholesterol,” and LDL cholesterol is dubbed, “the bad cholesterol.” However, there is nothing inherently bad about LDL cholesterol.
LDL cholesterol is critical to maintain life. It is created within the liver, and its purpose is to transport cholesterol to cells where it is used for important functions. It is needed by the body to make all the critical hormones in your body, including vitamin D. LDL cholesterol only becomes “bad,” or harmful, when it is damaged. LDL cholesterol is damaged by free radicals, which easily oxidize LDL cholesterol, but not HDL cholesterol.
Only damaged, or the oxidized form of LDL cholesterol sticks to the arterial walls to initiate the formation of plaque.(16) Studies reveal that those who have an increased percentage of atherosclerotic plaque are not necessarily those with a high LDL cholesterol level, but those with a higher percentage of oxidized LDL cholesterol than others. (1)
Low LDL Cholesterol Is Still Harmful …If Oxidized
 Only oxidized LDL cholesterol sticks to your arteries, causing inflammation and ultimately arterial plaque. If LDL cholesterol is not oxidized, or damaged, then it will not stick to your arterial walls or form plaque, …no matter the level. Low LDL cholesterol levels are still not safe if the oxidized LDL cholesterol percentage is elevated. Therefore, if you have a low LDL cholesterol you should not think you are not at risk for a heart attack. In addition, if your LDL cholesterol level that is too low you could develop health problems, in part due to lack of hormone production.
Only oxidized LDL cholesterol sticks to your arteries, causing inflammation and ultimately arterial plaque. If LDL cholesterol is not oxidized, or damaged, then it will not stick to your arterial walls or form plaque, …no matter the level. Low LDL cholesterol levels are still not safe if the oxidized LDL cholesterol percentage is elevated. Therefore, if you have a low LDL cholesterol you should not think you are not at risk for a heart attack. In addition, if your LDL cholesterol level that is too low you could develop health problems, in part due to lack of hormone production.
The key to lowering your risk of heart disease is lowering oxidized LDL cholesterol level, and elevating your HDL cholesterol level.
It is critical to understand that it is not simply the level of your LDL cholesterol that is the issue, it is actually the level of oxidized, or damaged LDL cholesterol that is of greatest concern. Cholesterol-lowering statin drugs do not address the true “bad cholesterol,” i.e., the oxidized LDL cholesterol level.
Relationship of LDL Cholesterol Level and Coronary Artery Disease
If you are told you have high LDL cholesterol, and you then take a statin drug to lower it, how much does it lower your risk of Coronary Artery Disease (CAD)? The answer: minimally. There is a small direct relationship between lowering your LDL cholesterol level and reducing your risk of CAD, as shown on the chart below. (2)
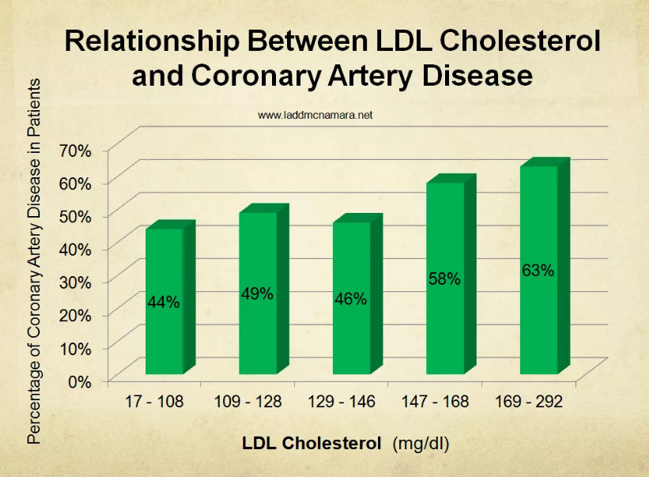
Now compare your risk of coronary artery disease and your level of oxidized LDL cholesterol. As you can see in the below graph, there is a direct and proportional relationship of the oxidized LDL level and the risk of CAD.
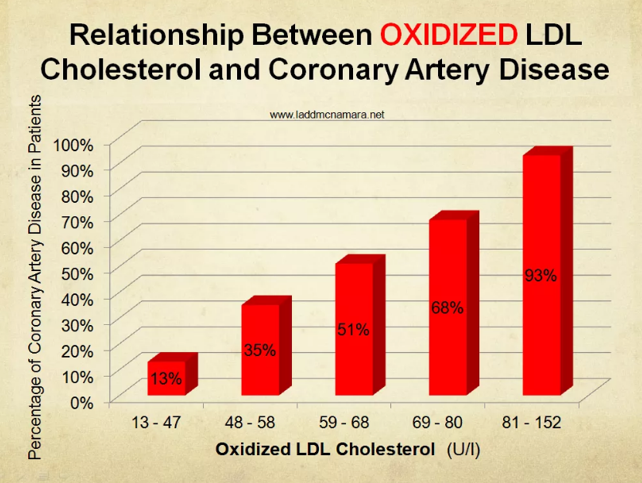
These charts show how important it is to know, and work to lower, your oxidized LDL level, regardless of your LDL level. So, if you have been struggling to lower your LDL cholesterol, or if your levels have increased after stopping a statin drug, then please understand that it is not necessary to be overly concerned about the actual level of LDL (in most cases), as long as your oxidized LDL cholesterol percentage is kept low; along with a reduction of arterial inflammation.
Oxidized LDL cholesterol is not checked on routine lipid panels. Your doctor may not have even heard of oxidized LDL cholesterol, yet it remains one of the main factors for the development of cardiovascular disease.
Lower Your Risk of Heart Attack and Heart Disease
The key to lowering your risk of heart disease is lowering oxidized LDL cholesterol level, and elevating your HDL cholesterol level. HDL, or high-density lipoprotein cholesterol, is responsible for clearing out excess cholesterol in your blood, and returning it to the liver for reprocessing. (Homocysteine and C reactive protein levels should also be kept low. All this is discussed at length within my audio book, The Cholesterol Conspiracy , as well as in my Dr. Ladd VIP Program where I give specific nutritional supplement suggestions for naturally improving all these parameters.)
 Exercise, vitamins, minerals, essential fatty acids (fish oil), and antioxidants, particularly the bioflavonoid antioxidants, increase HDL cholesterol levels and protect your LDL cholesterol from oxidative damage, arterial inflammation and plaque formation. (3) This means that you can actually reduce your risk of heart attack and heart disease by making these lifestyle modifications and taking nutritional supplements than you could by taking a statin drug.
Exercise, vitamins, minerals, essential fatty acids (fish oil), and antioxidants, particularly the bioflavonoid antioxidants, increase HDL cholesterol levels and protect your LDL cholesterol from oxidative damage, arterial inflammation and plaque formation. (3) This means that you can actually reduce your risk of heart attack and heart disease by making these lifestyle modifications and taking nutritional supplements than you could by taking a statin drug.
When choosing a quality nutritional supplement brand, be sure that it is potent, pure, and bio-available, and at doses that can truly make a difference.
References
- Anselmi M, et al. Plasma levels of oxidized-low-density lipoproteins are higher in patients with unstable angina and correlated with angiographic coronary complex plaques. Atherosclerosis. 2006 Mar;185(1):114-20.
- Johnston N, et al. Improved Identification of Patients With Coronary Artery Disease by the Use of New Lipid and Lipoprotein Biomarkers. Am J Cardiol. 2006 Mar 1;97(5):640-5.
- Aviram M. HDL–associated paraoxonase 1 (PON1) and dietaryantioxidants attenuate lipoprotein oxidation, macrophage foam cells formation and atherosclerosis development. Pathophysiol Haemost Thromb. 2006;35(1-2):146-51.
- Hoffman RM, et al. Antioxidants and the prevention of coronary heart disease. Arch Int Med. 1995 155:241-244.
- Levine GN, et al. Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996 93:6:1107-1113.
- Osganian S, Stampfer M, Rimm E, Spiegelman D, et al. Vitamin C and risk of coronary heart disease in women. J Am Coll Cardiol. 2003 42:246-252.
- Gaziano J. Antioxidant vitamins and coronary artery disease risk. Am J Med. 1994 97:3A-18S-3A-21S.
- Knekt P, et al. Flavonoid intake and coronary mortality in finland: a cohort study. Brit Med J. 1996 312:478-481.
- Niki E, et al. Interaction among vitamin C, vitamin E, and beta carotene. Am J Clin Nutri. 1995 62(suppl):1322S-1326S.
- Nestel P, et al. The n-3 fatty acids eiosapentaenoid acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr 2002 Aug;76(2):326-330.
- Hertog M, Feskens E, Hollman P, Katan M, Kromhout D. Dietary antioxidant flavonoids and risk of coronary heart disease: the Zutphen Elderly study. Lancet 1993 Oct 23;342(8878):1007-1011.
- Owen RW, et al. Olive oil consumption and health: the possible role of antioxidants. Lancet Oncol, 2000, Oct., 1:107-12.
- Visioli F., et al. Low density lipoprotein oxidation is inhibited in vitro by olive oil constituents. Atherosclerosis. 1995 Sep;117(1):25-32.
- Nagyova A, et al. Effects of dietary extra virgin olive oil on serum lipid resistance to oxidation and fatty acid composition in elderly lipidemic patients. Bratisl Lek Listy. 2003;104(7-8):218
- Visioli F., et al. Low density lipoprotein oxidation is inhibited in vitro by olive oil constituents. Atherosclerosis. 1995 Sep;117(1):25-32.
- Zhang WJ, Frei B. Alpha-lipoic acid inhibits TNF-alpha-induced NF-kappa B activation and adhesion molecule expression in human aortic endothelial cells. FASEB J 2001 Nov;15(13):2423-2432.
Copyright 2019, Ladd McNamara, Inc.



Thank you powerful information